Silambam Mastery
Remedies Asthma
Remedies Asthma
Asthma
Published: 22 November 2014
Last Updated: 15 May 2025 04:30 AM (GMT+8)
Bahasa Melayu : Asma/Lelah / Malayalam : ശ്വാസരോഗം (Shvaasarogam) / ശ്വാസംമുട്ടൽ (Shvaasammuttal) / Telugu : ఉబ్బసం (Ubbasaṁ) / Français : Asthme
Asthma Treatment
Asthma:
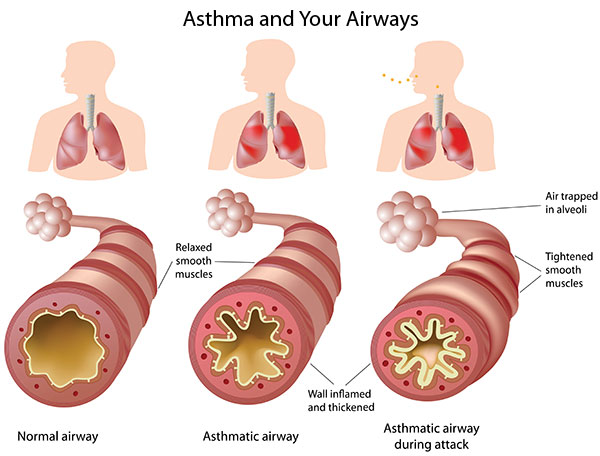
- Asthma is a condition in which the air passages in the lungs suddenly contract
- This reduces amount of air that can pass, making breathing difficult
Symptoms to look for:
- Breathlessness
- Pressure in the chest
- Cough
Causes:
- Allergic asthma is a result of body's reaction to allergens like
- Dust
- Smoke
- Drugs
- Pollution
- Causes of Non allergic asthma
- Fear
- Anxiety
- Stress
- Excessive consumption of processed food
- High salt intake
- Low intake of omega 3 fatty acids and anti oxidants
- Genetic factors
Natural home remedy using honey:
1. Fill a saucer with honey
2. Hold it beneath the nose and inhale
3. This helps to ease the breathing
Natural home remedy using fenugreek seeds, ginger and honey:
1. Take 2 tbsp of fenugreek seeds
2. Mix in 1 L of water
3. Let it simmer for 30 min
4. Strain the liquid
5. Crush ginger to make 2 tsp of ginger paste
6. Press the paste on a sieve and extract juice
7. Add ginger juice to the strained liquid
8. Add 1 tsp of honey
9. Mix well
10. Drink 1 glass of the mixture every morning
Natural home remedy using Indian gooseberry powder and honey:
1. Take 2 tsp of Indian gooseberry powder
2. You may de-seed and crush 1 Indian gooseberry and use it in place of the powder
3. Mix 1 tsp of honey
4. Have this once every morning
Tips:
- Breathe in clean air
- Wear a cloth mask
- Stay away from identified allergens
- Avoid pets which have feathers or fur
What is Asthma ?

Asthma is a commonly found disease which is chronic in nature and causes inflammatory disorders of a patients airways(passage through which air reaches the lungs of a human body). The type of health problems encountered due to such a condition by a person are attacks of wheezing, coughing, breathlessness and chest tightness.
Over the last four decades instances of asthma has multiplied significantly over the world, which can quite understandably be attributed to the explosion of pollution, population and contamination of nature by various man made activities. The graveness of the situation and the disease can be understood by the fact that 250000 deaths, globally, were reported in 2009 due to Asthma.
Causes of Asthma
Asthma is caused by environmental factors and may also be influenced by family history of this chronic disease. The symptoms are generally triggered by inhaling of allergy causing substances known as allergens. Following is the list of common allergens :
■ Dust
■ Animal hair ( usually of pets )
■ Exercises
■ Mold
■ Pollen
■ Weather changes
■ Respiratory infections like common cold
■ Emotional imbalances and stress
■ Smoking and usage of tobacco in various forms
In some patients asthma is also provoked by non-steroidal anti–inflammatory drugs like Aspirin.
Signs and Symptoms of Asthma
Asthma is characterized generally by coughing, wheezing and shortness of breath. The symptoms may vary where in the patient can have long term difficulty in breathing with sudden episodes of increased shortness of breathing. The Asthma attack scan last for few minutes or days and may be serious deserving urgent medical attention if airflow is severely blocked. Symptoms are listed as below.
■ Coughing, may be dry or with sputum.
■ Wheezing may be in various forms. It may come in episodes and normal in other times.
■ Shortness of breath which worsens with physical activity.
■ Abnormal breathing pattern.
■ Chest pain or tightness feeling in chest.
■ Flaring of nasal.
Different Types of Asthma Allergies
Clinically asthma is classified according to various factors such as frequency of symptoms, and the expiratory flow rates. Other factor of classification include a topic of non-atopic i.e. .whether the condition is invoked by allergens or not. Following are the few modes in which this can be classified.
■ Brittle asthma
Characterized by frequent severe attacks .This can appear in spite of intense medication in some cases.
■ Excercise induced Asthma
There has been a correlation that is discovered between exercise and the disease. Sports such as cycling, running and mountain biking are found to be more susceptible to the disease as found in certain studies.
■ Occupational Asthma
This kind of asthma is a very commonly reported occupational respiratory disease. This refers to the asthmatic condition that arises or worsens due to the exposures one has to face during his/her work hours. The highly impacted occupations under this category are operators, labourers and fabricators which mainly come under the canopy of the manufacturing industries. The exposure to animal proteins, enzymes, flour and chemicals are believed to be a high contributor to the work related asthma. Other occupations, such as management, sales or administrative jobs, though less severely hit, but do have substantial contribution to asthma.
Diagnosis of Asthma
Currently there is no precise medical test used to diagnose or confirm the presence of asthma in a patient. Rather, the approach that is mostly taken is based on the pattern of symptoms.
In many a cases, the health care specialist may suggest some therapy for some duration of time and then diagnose the problem as asthma if the patient responds positively to the medication.
Generally, the diagnosis comprises of assessing the following indicators
■ Wheezing –Whistling sounds usually of high pitched, when the patient exhales.
■ Family history of asthma attacks.
■ Frequent difficulty in breathing, recurrent coughing or feeling of chest pain or tightness.
Treatment for Asthma Allergies
In case avoiding the triggers only does not suffice, medical suggestions should be sought.
Medications used in asthma are classified in two categories.
■ Fast Acting.
These are quick relief drugs usually to be taken in acute conditions.. These medicines include inhalers (bronchodilators) such as salbutamol, proventil and ventolin. The doctor may prescribe some oral steroids comprising of pills or capsules in case the attack refuses to go and is very sever in nature.
■ Long term control.
This type of medication is to be used if the patient is not suffering from acute life threatening attacks, and aims at controlling the disease by taking the medicines for a longer period of time in a consistent manner. Corticosteroids, which are generally taken by inhaling are used which aim at preventing the air passage in the respiratory system from swelling up and thus blocking the airway. Long-acting beta-agonist inhalers also fall into this category which has generally effect tof at least 12 hours. Few other medications that fall under this category are Omalizumab and Cromolyn sodium (Intal) etc.
Home remedies & natural treatment for Asthma
A word derived from Greek etymology which literally means 'panting' or 'gasping' for breath; is attributed to a disease related to the respiratory tract. Triggered by way of an allergic reaction of the body to one or many stimulants or 'allergens'; a patient in its attacking spell suffers from breathlessness. Marked by a prolonged difficulty in breathing out, asthma is marked by involuntary spasm of small muscular air passages of lungs. Occurring primarily due to an allergic reaction a number of triggers or irritants including those from weather, food, medication and use or exposure to certain chemicals may mark the onset of asthmatic attack.
For effective control and remedy of asthma; one needs to ascertain the allergen or irritant which triggers such an attack. Thus controlling the conditions which account for asthma will indirectly lead to fewer attacks of asthma.
Home Remedy For Asthma - Effective Natural Asthma Treatment
■ For people susceptible to asthma on account of pollen, dust and pets need to ensure their protection against the causal factors. It is imperative that they go for air conditioning of their rooms and cars to prevent exposure to the sources of irritation.
■ It is imperative that they stay away from carpets, draperies and toys which accumulate dust. The ones allergic to animal furs need to ensure that pets are not allowed in vicinity of living rooms.
■ Besides avoiding the likely allergens, certain dietary means have been found beneficial for those prone to asthmatic attacks. For instance powdered turmeric added to milk keeps such attacks away; if consumed daily on empty stomach.
■ Five to six cloves boiled in half a glass of water with a spoon full of honey serve as an excellent decoction against asthma; if taken twice a day.
■ Crushed cloves of garlic may be boiled in six tea spoons of milk for regular consumption of the same by an asthma prone person.
■ Regular exposure to fresh air and sun light free from pollutants contributed by factories and means of transport is also important in order to counter the attacks of asthma.
■ One of the naturally effective home remedies include a decoction including tea spoon full measures of raw honey, ginger powder and ground black pepper.
■ Dried grapes soaked in water and then in cold milk may be had on an empty stomach in order to counter asthmatic attacks. Consumption of grapes serves to strengthen lungs and flush the toxic contents of human body.
■ Dried figs also serve to flush out the phlegm content of the respiratory tract.
■ Equal measures of honey and olive oil may be added to warm milk. The consumption of the resulting milk along with a few cloves of garlic before breakfast acts as an antidote to asthmatic attacks.
■ Half a glass measure of boiled fenugreek juice along with tea spoons measure of ginger juice is also an excellent natural remedy. It serves to decongest and detoxify the lungs.
■ Regular consumption of fennel seeds also has a similar purpose to serve.
■ Herbal tea with ground ginger and a dash of lime juice is also effective. Patients susceptible to asthmatic attacks may choose the same over milk tea to be consumed twice a day. Herbal tea based on licorice root is extremely beneficial.
■ Turmeric and honey taken separately early in the morning keeps you away from the painful bouts of asthmatic attacks.
■ Crushed gooseberry in a table spoon of honey also serves as a natural remedial medicine.
■ Soup made out of radish, honey and lemon juice may be made by blending the mentioned ingredients. Regular consumption of at least ten grams the same mixture is beneficial for asthma patients. Both the medicinally enriched natural ingredients will serve to excrete mucus and detoxify the respiratory tract.
■ Broth made out of leaves of drumstick is equally helpful for patients afflicted with asthma.
■ Juice of bitter gourd added to honey and paste of basil also ranks amongst the numerous natural options. Spoon full of the same serves to defend yourself from asthmatic attacks.
■ Dried pomegranates and raisins boiled in milk also serve to be an effective remedial measure.
■ Dried and powdered seeds of safflower acts as a natural expectorant if consumed with a spoon full measure of honey.
■ In case one finds himself in the grip of an attack warm mustard oil with a bit of crushed camphor should be massaged on the victim's back and chest to make way for ease in breathing.
■ Inhaling of steam from water boiled in 'ajwain' seeds will also prove to be relieving.
■ Inhaling steam from water enriched with herbal oil of 'juniper' may be another relieving option.
■ Inhaling the smell of honey is also said to be similarly beneficial.
Apart from adopting a dietary regimen insisting on fruits, vegetable and honey; patients susceptible to breathing spasms on account of asthma should be cautious about his weight. Special medical advice and care should be taken as to the use of humidifiers and inhalers if the bouts of attack are frequent.
ICD-10 J45
ICD-9 493
OMIM 600807
DiseasesDB 1006
MedlinePlus 000141
eMedicine article/806890
MeSH D001249
Asthma (from the Greek ἅσθμα, ásthma, "panting") is a common chronic inflammatory disease of the airways characterized by variable and recurring symptoms, reversible airflow obstruction, and bronchospasm. Common symptoms include wheezing, coughing, chest tightness, and shortness of breath.
Asthma is thought to be caused by a combination of genetic and environmental factors. Its diagnosis is usually based on the pattern of symptoms, response to therapy over time, and spirometry. It is clinically classified according to the frequency of symptoms, forced expiratory volume in one second (FEV1), and peak expiratory flow rate. Asthma may also be classified as atopic (extrinsic) or non-atopic (intrinsic) where atopy refers to a predisposition toward developing type 1 hypersensitivity reactions.
Treatment of acute symptoms is usually with an inhaled short-acting beta-2 agonist (such as salbutamol) and oral corticosteroids. In very severe cases, intravenous corticosteroids, magnesium sulfate, and hospitalization may be required. Symptoms can be prevented by avoiding triggers, such as allergens and irritants, and by the use of inhaled corticosteroids. Long-acting beta agonists (LABA) or leukotriene antagonists may be used in addition to inhaled corticosteroids if asthma symptoms remain uncontrolled. The prevalence of asthma has increased significantly since the 1970s. In 2011, 235–300 million people globally have been diagnosed with asthma, and it caused 250,000 deaths.
Signs and symptoms
Asthma is characterized by recurrent episodes of wheezing, shortness of breath, chest tightness, and coughing. Sputum may be produced from the lung by coughing but is often hard to bring up. During recovery from an attack it may appear pus like due to high levels of white blood cells called eosinophils. Symptoms are usually worse at night and in the early morning or in response to exercise or cold air. Some people with asthma rarely experience symptoms, usually in response to triggers, whereas others may have marked and persistent symptoms.
Associated conditions
A number of other health conditions occur more frequently in those with asthma, including gastro-esophageal reflux disease (GERD), rhinosinusitis, and obstructive sleep apnea. Psychological disorders are also more common, with anxiety disorders occurring in between 16–52% and mood disorders in 14–41%. However, it is not known if asthma causes psychological problems or if psychological problems lead to asthma.
Causes
Asthma is caused by a combination of complex and incompletely understood environmental and genetic interactions. These factors influence both its severity and its responsiveness to treatment. It is believed that the recent increased rates of asthma are due to changing epigenetics (heritable factors other than those related to the DNA sequence) and a changing living environment.
Environmental
Many environmental factors have been associated with asthma's development and exacerbation including allergens, air pollution, and other environmental chemicals. Smoking during pregnancy and after delivery is associated with a greater risk of asthma-like symptoms. Low air quality from factors such as traffic pollution or high ozone levels, has been associated with both asthma development and increased asthma severity. Exposure to indoor volatile organic compounds may be a trigger for asthma; formaldehyde exposure, for example, has a positive association. Also, phthalates in PVC are associated with asthma in children and adults as are high levels of endotoxin exposure.
Asthma is associated with exposure to indoor allergens. Common indoor allergens include: dust mites, cockroaches, animal dander, and mold. Efforts to decrease dust mites have been found to be ineffective. Certain viral respiratory infections, such as respiratory syncytial virus and rhinovirus, may increase the risk of developing asthma when acquired as young children. Certain other infections, however, may decrease the risk.
Hygiene hypothesis
The hygiene hypothesis attempts to explain the increased rates of asthma worldwide as a direct and unintended result of reduced exposure, during childhood, to non-pathogenic bacteria and viruses. It has been proposed that the reduced exposure to bacteria and viruses is due, in part, to increased cleanliness and decreased family size in modern societies. Evidence supporting the hygiene hypothesis includes lower rates of asthma on farms and in households with pets.
Use of antibiotics in early life has been linked to the development of asthma. Also, delivery via caesarean section is associated with an increased risk (estimated at 20–80%) of asthma—this increased risk is attributed to the lack of healthy bacterial colonization that the newborn would have acquired from passage through the birth canal. There is a link between asthma and the degree of affluence.
Genetic
CD14-endotoxin interaction based on CD14 SNP C-159T :
Endotoxin levels CC genotype TT genotype
High exposure Low risk High risk
Low exposure High risk Low risk
Family history is a risk factor for asthma, with many different genes being implicated. If one identical twin is affected, the probability of the other having the disease is approximately 25%. By the end of 2005, 25 genes had been associated with asthma in six or more separate populations, including GSTM1, IL10, CTLA-4, SPINK5, LTC4S, IL4R and ADAM33, among others. Many of these genes are related to the immune system or modulating inflammation. Even among this list of genes supported by highly replicated studies, results have not been consistent among all populations tested. In 2006 over 100 genes were associated with asthma in one genetic association study alone; more continue to be found.
Some genetic variants may only cause asthma when they are combined with specific environmental exposures. An example is a specific single nucleotide polymorphism in the CD14 region and exposure to endotoxin (a bacterial product). Endotoxin exposure can come from several environmental sources including tobacco smoke, dogs, and farms. Risk for asthma, then, is determined by both a person's genetics and the level of endotoxin exposure.
Medical conditions
A triad of atopic eczema, allergic rhinitis and asthma is called atopy. The strongest risk factor for developing asthma is a history of atopic disease; with asthma occurring at a much greater rate in those who have either eczema or hay fever. Asthma has been associated with Churg–Strauss syndrome, an autoimmune disease and vasculitis. Individuals with certain types of urticaria may also experience symptoms of asthma.
There is a correlation between obesity and the risk of asthma with both having increased in recent years. Several factors may be at play including decreased respiratory function due to a buildup of fat and the fact that adipose tissue leads to a pro-inflammatory state.
Beta blocker medications such as propranolol can trigger asthma in those who are susceptible. Cardioselective beta-blockers, however, appear safe in those with mild or moderate disease. Other medications that can cause problems are ASA, NSAIDs, and angiotensin-converting enzyme inhibitors.
Exacerbation
Some individuals will have stable asthma for weeks or months and then suddenly develop an episode of acute asthma. Different individuals react differently to various factors. Most individuals can develop severe exacerbation from a number of triggering agents.
Home factors that can lead to exacerbation of asthma include dust, animal dander (especially cat and dog hair), cockroach allergens and mold. Perfumes are a common cause of acute attacks in women and children. Both viral and bacterial infections of the upper respiratory tract can worsen the disease. Psychological stress may worsen symptoms—it is thought that stress alters the immune system and thus increases the airway inflammatory response to allergens and irritants.
Pathophysiology
Asthma is the result of chronic inflammation of the airways which subsequently results in increased contractability of the surrounding smooth muscles. This among other factors leads to bouts of narrowing of the airway and the classic symptoms of wheezing. The narrowing is typically reversible with or without treatment. Occasionally the airways themselves change. Typical changes in the airways include an increase in eosinophils and thickening of the lamina reticularis. Chronically the airways' smooth muscle may increase in size along with an increase in the numbers of mucous glands. Other cell types involved include: T lymphocytes, macrophages, and neutrophils. There may also be involvement of other components of the immune system including: cytokines, chemokines, histamine, and leukotrienes among others.
Diagnosis
While asthma is a well recognized condition, there is not one universal agreed upon definition. It is defined by the Global Initiative for Asthma as "a chronic inflammatory disorder of the airways in which many cells and cellular elements play a role. The chronic inflammation is associated with airway hyper-responsiveness that leads to recurrent episodes of wheezing, breathlessness, chest tightness and coughing particularly at night or in the early morning. These episodes are usually associated with widespread but variable airflow obstruction within the lung that is often reversible either spontaneously or with treatment".
There is currently no precise test with the diagnosis typically based on the pattern of symptoms and response to therapy over time. A diagnosis of asthma should be suspected if there is a history of: recurrent wheezing, coughing or difficulty breathing and these symptoms occur or worsen due to exercise, viral infections, allergens or air pollution. Spirometry is then used to confirm the diagnosis. In children under the age of six the diagnosis is more difficult as they are too young for spirometry.
Spirometry
Spirometry is recommended to aid in diagnosis and management. It is the single best test for asthma. If the FEV1 measured by this technique improves more than 12% following administration of a bronchodilator such as salbutamol, this is supportive of the diagnosis. It however may be normal in those with a history of mild asthma, not currently acting up. As caffeine is a bronchodilator in people with asthma, the use of caffeine before a lung function test may interfere with the results. Single-breath diffusing capacity can help differentiate asthma from COPD. It is reasonable to perform spirometry every one or two years to follow how well a person's asthma is controlled.
Others
The methacholine challenge involves the inhalation of increasing concentrations of a substance that causes airway narrowing in those predisposed. If negative it means that a person does not have asthma; if positive, however, it is not specific for the disease.
Other supportive evidence includes: a ≥20% difference in peak expiratory flow rate on at least three days in a week for at least two weeks, a ≥20% improvement of peak flow following treatment with either salbutamol, inhaled corticosteroids or prednisone, or a ≥20% decrease in peak flow following exposure to a trigger. Testing peak expiratory flow is more variable than spirometry, however, and thus not recommended for routine diagnosis. It may be useful for daily self-monitoring in those with moderate to severe disease and for checking the effectiveness of new medications. It may also be helpful in guiding treatment in those with acute exacerbations.
Classification
Clinical classification (≥ 12 years old)
Severity Symptom frequency Night time symptoms %FEV1 of predicted FEV1 Variability SABA use
Intermittent ≤2/week ≤2/month ≥80% <20% ≤2 days/week
Mild persistent >2/week 3–4/month ≥80% 20–30% >2 days/week
Moderate persistent Daily >1/week 60–80% >30% daily
Severe persistent Continuously Frequent (7×/week) <60% >30% ≥twice/day
Asthma is clinically classified according to the frequency of symptoms, forced expiratory volume in one second (FEV1), and peak expiratory flow rate. Asthma may also be classified as atopic (extrinsic) or non-atopic (intrinsic), based on whether symptoms are precipitated by allergens (atopic) or not (non-atopic). While asthma is classified based on severity, at the moment there is no clear method for classifying different subgroups of asthma beyond this system. Finding ways to identify subgroups that respond well to different types of treatments is a current critical goal of asthma research.
Although asthma is a chronic obstructive condition, it is not considered as a part of chronic obstructive pulmonary disease as this term refers specifically to combinations of disease that are irreversible such as bronchiectasis, chronic bronchitis, and emphysema. Unlike these diseases, the airway obstruction in asthma is usually reversible; however, if left untreated, the chronic inflammation from asthma can lead the lungs to become irreversibly obstructed due to airway remodeling. In contrast to emphysema, asthma affects the bronchi, not the alveoli.
Asthma exacerbation
An acute asthma exacerbation is commonly referred to as an asthma attack. The classic symptoms are shortness of breath, wheezing, and chest tightness. While these are the primary symptoms of asthma, some people present primarily with coughing, and in severe cases, air motion may be significantly impaired such that no wheezing is heard.
Signs which occur during an asthma attack include the use of accessory muscles of respiration (sternocleidomastoid and scalene muscles of the neck), there may be a paradoxical pulse (a pulse that is weaker during inhalation and stronger during exhalation), and over-inflation of the chest. A blue color of the skin and nails may occur from lack of oxygen.
In a mild exacerbation the peak expiratory flow rate (PEFR) is ≥200 L/min or ≥50% of the predicted best. Moderate is defined as between 80 and 200 L/min or 25% and 50% of the predicted best while severe is defined as ≤ 80 L/min or ≤25% of the predicted best.
Acute severe asthma, previously known as status asthmaticus, is an acute exacerbation of asthma that does not respond to standard treatments of bronchodilators and corticosteroids. Half of cases are due to infections with others caused by allergen, air pollution, or insufficient or inappropriate medication use.
Brittle asthma is a kind of asthma distinguishable by recurrent, severe attacks. Type 1 brittle asthma is a disease with wide peak flow variability, despite intense medication. Type 2 brittle asthma is background well-controlled asthma with sudden severe exacerbations.
Exercise-induced
Exercise can trigger bronchoconstriction in both people with and without asthma. It occurs in most people with asthma and up to 20% of people without asthma. In athletes is diagnosed more commonly in elite athletes, with rates varying from 3% for bobsled racers to 50% for cycling and 60% for cross-country skiing. While it may occur with any weather conditions it is more common when it is dry and cold. Inhaled beta2-agonists do not appear to improve athletic performance among those without asthma however oral doses may improve endurance and strength.
Occupational
Asthma as a result of (or worsened by) workplace exposures, is a commonly reported occupational disease. Many cases however are not reported or recognized as such. It is estimated that 5–25% of asthma cases in adults are work–related. A few hundred different agents have been implicated with the most common being: isocyanates, grain and wood dust, colophony, soldering flux, latex, animals, and aldehydes. The employment associated with the highest risk of problems include: those who spray paint, bakers and those who process food, nurses, chemical workers, those who work with animals, welders, hairdressers and timber workers.
Differential diagnosis
Many other conditions can cause symptoms similar to those of asthma. In children, other upper airway diseases such as allergic rhinitis and sinusitis should be considered as well as other causes of airway obstruction including: foreign body aspiration, tracheal stenosis or laryngotracheomalacia, vascular rings, enlarged lymph nodes or neck masses. In adults, COPD, congestive heart failure, airway masses, as well as drug-induced coughing due to ACE inhibitors should be considered. In both populations vocal cord dysfunction may present similarly.
Chronic obstructive pulmonary disease can coexist with asthma and can occur as a complication of chronic asthma. After the age of 65 most people with obstructive airway disease will have asthma and COPD. In this setting, COPD can be differentiated by increased airway neutrophils, abnormally increased wall thickness, and increased smooth muscle in the bronchi. However, this level of investigation is not performed due to COPD and asthma sharing similar principles of management: corticosteroids, long acting beta agonists, and smoking cessation. It closely resembles asthma in symptoms, is correlated with more exposure to cigarette smoke, an older age, less symptom reversibility after bronchodilator administration, and decreased likelihood of family history of atopy.
Prevention
The evidence for the effectiveness of measures to prevent the development of asthma is weak. Some show promise including: limiting smoke exposure both in utero and after delivery, breastfeeding, and increased exposure to daycare or large families but none are well supported enough to be recommended for this indication. Early pet exposure may be useful. Results from exposure to pets at other times are inconclusive and it is only recommended that pets be removed from the home if a person has allergic symptoms to said pet. Dietary restrictions during pregnancy or when breast feeding have not been found to be effective and thus are not recommended. Reducing or eliminating compounds known to sensitive people from the work place may be effective.
Management
While there is no cure for asthma, symptoms can typically be improved. A specific, customized plan for proactively monitoring and managing symptoms should be created. This plan should include the reduction of exposure to allergens, testing to assess the severity of symptoms, and the usage of medications. The treatment plan should be written down and advise adjustments to treament according to changes in symptoms.
The most effective treatment for asthma is identifying triggers, such as cigarette smoke, pets, or aspirin, and eliminating exposure to them. If trigger avoidance is insufficient, the use of medication is recommended. Pharmaceutical drugs are selected based on, among other things, the severity of illness and the frequency of symptoms. Specific medications for asthma are broadly classified into fast-acting and long-acting categories.
Bronchodilators are recommended for short-term relief of symptoms. In those with occasional attacks, no other medication is needed. If mild persistent disease is present ( more than two attacks a week ), low-dose inhaled corticosteroids or alternatively, an oral leukotriene antagonist or a mast cell stabilizer is recommended. For those who have daily attacks, a higher dose of inhaled corticosteroids is used. In a moderate or severe exacerbation, oral corticosteroids are added to these treatments.
Lifestyle modification
Avoidance of triggers is a key component of improving control and preventing attacks. The most common triggers include allergens, smoke (tobacco and other), air pollution, non selective beta-blockers, and sulfite-containing foods. Cigarette smoking and second-hand smoke (passive smoke) may reduce the effectiveness of medications such as corticosteroids. Dust mite control measures, including air filtration, chemicals to kill mites, vacuuming, mattress covers and others methods had no effect on asthma symptoms. Overall exercise, however is beneficial in people with stable asthma.
Medications
Medications used to treat asthma are divided into two general classes: quick-relief medications used to treat acute symptoms; and long-term control medications used to prevent further exacerbation.
Fast–acting
-Short-acting beta2-adrenoceptor agonists (SABA), such as salbutamol (albuterol USAN) are the first line treatment for asthma symptoms. They are recommended before exercise in those with exercise induced symptoms.
-Anticholinergic medications, such as ipratropium bromide, provide additional benefit when used in combination with SABA in those with moderate or severe symptoms. Anticholinergic bronchodilators can also be used if a person cannot tolerate a SABA.
-Older, less selective adrenergic agonists, such as inhaled epinephrine, have similar efficacy to SABAs. They are however not recommended due to concerns regarding excessive cardiac stimulation.
Long–term control
-Corticosteroids are generally considered the most effective treatment available for long-term control. Inhaled forms such as beclomethasone are usually used except in the case of severe persistent disease, in which oral corticosteroids may be needed. It is usually recommended that inhaled formulations be used once or twice daily, depending on the severity of symptoms.
-Long-acting beta-adrenoceptor agonists (LABA) such as salmeterol and formoterol can improve asthma control, at least in adults, when given in combination with inhaled corticosteroids. In children this benefit is uncertain. When used without steroids they increase the risk of severe side-effects and even with corticosteroids they may slightly increase the risk.
-Leukotriene antagonists (such as montelukast and zafirlukast) may be used in addition to inhaled corticosteroids, typically also in conjunction with LABA. Evidence is insufficient to support use in acute exacerbations. In children under five years of age, they are the preferred add-on therapy after inhaled corticosteroids.
-Mast cell stabilizers (such as cromolyn sodium) are another non-preferred alternative to corticosteroids.
Delivery methods
Medications are typically provided as metered-dose inhalers (MDIs) in combination with an asthma spacer or as a dry powder inhaler. The spacer is a plastic cylinder that mixes the medication with air, making it easier to receive a full dose of the drug. A nebulizer may also be used. Nebulizers and spacers are equally effective in those with mild to moderate symptoms however insufficient evidence is available to determine whether or not a difference exists in those severe symptomatology.
Adverse effects
Long-term use of inhaled corticosteroids at conventional doses carries a minor risk of adverse effects. Risks include the development of cataracts and a mild regression in stature.
Others
When asthma is unresponsive to usual medications, other options are available for both emergency management and prevention of flareups. For emergency management other options include:
-Oxygen to alleviate hypoxia if saturations fall below 92%.
-Magnesium sulfate intravenous treatment has been shown to provide a bronchodilating effect when used in addition to other treatment in severe acute asthma attacks.
-Heliox, a mixture of helium and oxygen, may also be considered in severe unresponsive cases.
-Intravenous salbutamol is not supported by available evidence and is thus used only in extreme cases.
-Methylxanthines (such as theophylline) were once widely used, but do not add significantly to the effects of inhaled beta-agonists. Their use in acute exacerbations is controversial.
-The dissociative anesthetic ketamine is theoretically useful if intubation and mechanical ventilation is needed in people who are approaching respiratory arrest; however, there is no evidence from clinical trials to support this.
For those with severe persistent asthma not controlled by inhaled corticosteroids and LABAs bronchial thermoplasty may be an option. It involves the delivery of controlled thermal energy to the airway wall during a series of bronchoscopies. While it may increase exacerbation frequency in the first few months it appears to decrease the subsequent rate. Effects beyond one year are unknown. Evidence suggests that sublingual immunotherapy in those with both allergic rhinitis and asthma improve outcomes.
Alternative medicine
Many people with asthma, like those with other chronic disorders, use alternative treatments; surveys show that roughly 50% use some form of unconventional therapy. There is little data to support the effectiveness of most of these therapies. Evidence is insufficient to support the usage of Vitamin C. Acupuncture is not recommended for the treatment as there is insufficient evidence to support its use. Air ionisers show no evidence that they improve asthma symptoms or benefit lung function; this applied equally to positive and negative ion generators.
"Manual therapies", including osteopathic, chiropractic, physiotherapeutic and respiratory therapeutic maneuvers, have insufficient evidence to support their use in treating asthma. The Buteyko breathing technique for controlling hyperventilation may result in a reduction in medications use however does not have any effect on lung function. Thus an expert panel felt that evidence was insufficient to support its use.
Prognosis
The prognosis for asthma is generally good, especially for children with mild disease. Mortality has decreased over the last few decades due to better recognition and improvement in care. Globally it causes moderate or severe disability in 19.4 million people as of 2004 (16 million of which are in low and middle income countries). Of asthma diagnosed during childhood, half of cases will no longer carry the diagnosis after a decade. Airway remodeling is observed, but it is unknown whether these represent harmful or beneficial changes. Early treatment with corticosteroids seems to prevent or ameliorates a decline in lung function.
Epidemiology
As of 2011, 235–330 million people worldwide are affected by asthma, and approximately 250,000 people die per year from the disease. Rates vary between countries with prevalences between 1 and 18%. It is more common in developed than developing countries. One thus sees lower rates in Asia, Eastern Europe and Africa. Within developed countries it is more common in those who are economically disadvantaged while in contrast in developing countries it is more common in the affluent. The reason for these differences is not well known. Low and middle income countries make up more than 80% of the mortality.
While asthma is twice as common in boys as girls, severe asthma occurs at equal rates. In contrast adult women have a higher rate of asthma than men and it is more common in the young than the old.
Global rates of asthma have increased significantly between the 1960s and 2008 with it being recognized as a major public health problem since the 1970s. Rates of asthma have plateaued in the developed world since the mid-1990s with recent increases primarily in the developing world. Asthma affects approximately 7% of the population of the United States and 5% of people in the United Kingdom. Canada, Australia and New Zealand have rates of about 14–15%.
History
Asthma was recognized in Ancient Egypt and was treated by drinking an incense mixture known as kyphi. It was officially named as a specific respiratory problem by Hippocrates circa 450 BC, with the Greek word for "panting" forming the basis of our modern name. In 200 BC it was believed to be at least partly related to the emotions.
In 1873, one of the first papers in modern medicine on the subject tried to explain the pathophysiology of the disease while one in 1872, concluded that asthma can be cured by rubbing the chest with chloroform liniment. Medical treatment in 1880, included the use of intravenous doses of a drug called pilocarpin. In 1886, F.H. Bosworth theorized a connection between asthma and hay fever. Epinephrine was first referred to in the treatment of asthma in 1905. Oral corticosteroids began to be used for this condition in the 1950s while inhaled corticosteroids and selective short acting beta agonist came into wide use in the 1960s.
During the 1930s–1950s, asthma was known as one of the "holy seven" psychosomatic illnesses. Its cause was considered to be psychological, with treatment often based on psychoanalysis and other talking cures. As these psychoanalysts interpreted the asthmatic wheeze as the suppressed cry of the child for its mother, they considered the treatment of depression to be especially important for individuals with asthma.
nbsp;
|
Head |
|
|---|---|
|
Neck |
|
( including LRTIs )
|
Bronchial / obstructive |
| ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Interstitial / restrictive ( fibrosis ) |
| ||||||||||||||||
|
Obstructive or restrictive |
|
mediastinum
|
Pleural disease |
|
|---|---|
|
Mediastinal disease |
|
- Respiratory failure
- Influenza
- SARS
- Idiopathic pulmonary haemosiderosis
- Pulmonary alveolar proteinosis
Silambam Asia (SILA) is in official partnership with the United Nations Sustainable Development Goals (UN-SDGS) to preserve and safeguard the Indian traditional arts, sports, cultural, and educational content of Silambam at the international level.
Silambam Asia plays active roles as an international organization for governance and sustainable development in the Indian traditional arts and sports for education, health, fitness, culture, nature, climate change, recreation, and dissemination of all these related information. Thus, it is vital to provide expertise for members by providing training, research, revive, rejuvenate, retain, and restore.
The mission of Silambam Asia is to provide effective international governance by constantly improving technical rules and regulating Silambam competitions or participation in international events or sporting arenas to be recognized as an Olympic and Paralympic sport in the near future.
Silambam Asia - Introduction
Indian traditional arts and sports for education, health, fitness, culture, nature, climate change, recreation, and dissemination.
Video content with development work, achievements and silambam history.
We Support